The different classes of in vitro diagnostic medical devices (IVD-MDs)
A specific goal leading to a specific classification
Date
03/02/2023
A specific goal leading to a specific classification
Date
03/02/2023
In 2021, over 500 French companies were producing IVDDs, employing around 22,000 people, according to the Syndicat National de l'Industrie des Technologies Médicales (SNITEM).
Like “simple” medical devices, IVDDs help diagnose specific pathologies and contribute to patient care.
They are all around us, and we use them regularly without even realizing it. Very recently, we have witnessed the almost daily and massive use of IVDDs - PCR, antigenic and serological tests for COVID-19.
What exactly is an IVDD?
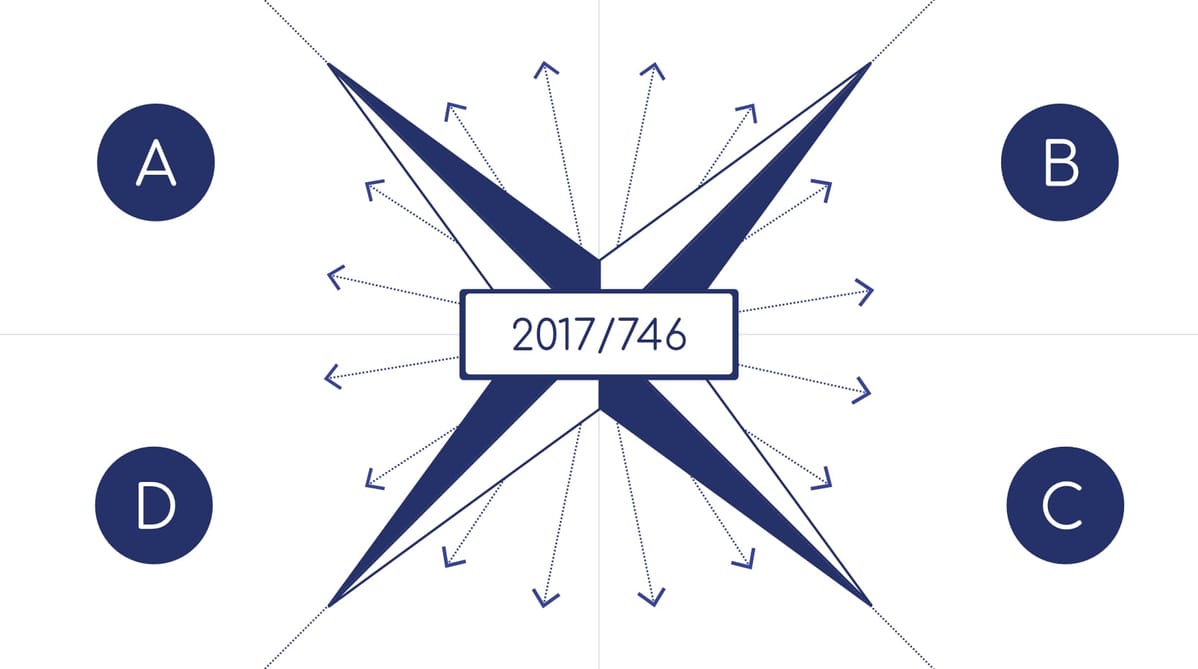
Regulation (EU) 2017/746 (IVDR) –Chap I, section 1 art. 2 gives us a detailed definition:
“Any medical device that consists of a reagent, reagent product, calibration material, control material, kit, instrument, apparatus, equipment, software or system, used alone or in combination, intended by the manufacturer to be used in vitro in the examination of samples from the human body, including donated blood and tissue, solely or principally for the purpose of providing information about one or more of the following:
a) concerning a physiological or pathological process or state;
b) concerning congenital physical or mental deficiencies;
c) concerning the predisposition to an affection or disease
d) determining whether a given treatment is safe for and compatible with potential recipients;
e) predicting response or reactions to a treatment;
f) to define or control therapeutic measures.
Sample containers are also considered to be in vitro diagnostic medical devices.
Not all IVDDs are on the same footing: for example, the stakes involved in taking a COVID self-test or a test to diagnose a transmissible agent of a high-risk disease (e.g. Ebola) are not proportional. The requirements for limiting the risk and ensuring the reliability of these two in-vitro diagnostic medical devices will therefore not be the same either.
What are the different classes of IVDDs?
IVDDs are classified into 4 classes according to the level of risk associated with their use:
It is the manufacturer's responsibility to determine the class of his medical device according to the medical purpose it aims to be used.
Identifying the class of a medical device is crucial to its further development and market access. A wrong initial positioning would imply longer compliance times, or even the impossibility of market access.
So-called “simple” medical devices (MD) have a specific classification and fall within a separate regulatory reference framework ((EU) MDR 2017/745)
What criteria should be used to identify the class of IVDD and meet regulatory requirements?
IVDD classification rules are defined by 7 rules in Regulation (EU) 2017/746.
IVDDs are classified according to several factors including:
The impact of classification on the CE marking procedure
The procedure for obtaining CE marking, whatever the class, requires 3 key elements to be put in place, just as for “simple” DM:
For non-sterile class A IVDDs, CE marking is obtained through self-certification by the manufacturer. In this case, the manufacturer must meet the requirements for its product, and put in place the necessary means to ensure its performance and safety.
For all other classes, CE certification is issued by a notified body following one or more audits to assess product compliance.
Obtaining CE certification is a major challenge for DM manufacturers
Essential
IVDDs (In-Vitro Diagnostic Medical Devices) are designed for the in vitro analysis of samples from the human body, in order to provide information on a person's physiological and pathological state (this includes equipment such as pregnancy tests, glucose analyzers, cholesterol tests, reagents for laboratory analyses, etc.).
They are classified into 4 classes (A to D) according to their specific features and level of risk.
Identifying the class of a medical device is decisive for its further development and market access. A wrong initial positioning would imply longer compliance times, or even the impossibility of market access.
This article is provided for information purposes only and does not constitute a normative or regulatory reference.